Elder care, up close and personal

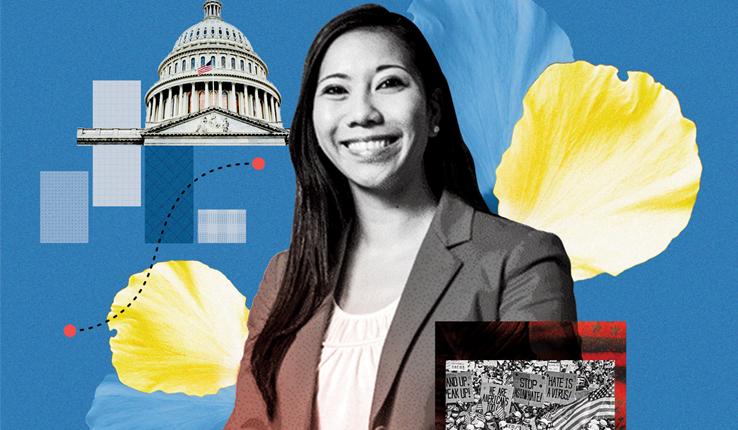
Olson (left), with her mother, Dorothy Katz, says elder care in America is plagued by sub-standard conditions and barriers to access.
For more than 35 years Laura Katz Olson has studied the impact of elder care policy on vulnerable populations in the United States. But not even her deep knowledge of the subject could prepare her for the elder care system she encountered when her own aging mother, Dorothy Katz, became incapacitated by Parkinson’s disease and a gradual loss of vision and required full-time care.
Olson says sub-standard conditions and barriers to accessing services typify elder care. Her first-hand experience of these as she helped her mother increased her determination to shed light on what she calls the nation’s high-priced, dysfunctional system of long-term care—funded by taxpayer dollars—that benefits private industry at the expense of the elderly.
Olson, a professor of political science, combines her policy expertise with her personal story in her latest book, Elder Care Journey, A View from the Front Lines (SUNY Press), which documents the demands and stresses of caregiving as well as the manifold indignities perpetrated by social welfare policy.
In the prologue, she writes: “Now that I have a front-row seat, it is obvious that my previous work had just skimmed the surface. It was as though I were now witnessing the access, cost and quality questions of health and long-term care through a magnifying glass.”
Unwarranted hurdles, appalling care
Olson knew from her work how unreasonable the bureaucratic welfare system was, but it was much worse than she had imagined.
“You are guilty until proven innocent,” says Olson, explaining the assumption with which she and her mother were met as they applied for benefits for low-income households. “The burden of proof is on the applicant, even if you are old and disabled.”
She explains: “I was forced to fill out form after form and produce difficult-to-obtain documentation, year after year, for every single service or subsidy she required. When there were snags—a frequent occurrence—I had to contend with standardized letters, hour-long waits on automated phone lines, and faceless (generally clueless) agents. Despite my ‘expertise’ in long-term care, I was often inundated with a sense of helplessness at the unwarranted hurdles that prevented my mother from acquiring vital services—and in a timely manner.”
But ultimately it was the treatment her mother received that was most appalling.
“Despite my grasp of nursing home failings, it took me aback to personally witness the negligent and appalling treatment my mother received in two Florida facilities for post-acute care; nothing could have prepared me for the indifference to her physical and cognitive needs, unpalatable meals, disdain for government regulations, and slapdash approach to patient care generally,” says Olson.
Olson does acknowledge that despite their discouraging experiences, she and her mother encountered people along the way who were caring and effectively serving older people in need.
For example, her mother now resides in a Pennsylvania nursing home where attentive and hard-working nurses and aides provide good enough care that Olson is no longer fearful for her mother’s health and safety.
A common experience
One might wish to assume that Olson’s experience is the exception. Unfortunately, her research says otherwise. The high cost of Long-Term Services and Supports (LTSS)—a Medicaid designation describing acute and long-term care services—far exceeds what most seniors are able to pay, she says.
According to the SCAN Foundation, an independent public charity dedicated to improving elder care, in 2012 the median annual cost of a nursing home stay (for a semi-private room) was $73,000 and $39,600 at an assisted living facility. Caring for a loved one at home is also costly with the median price tag for home health and personal services totaling $43,472.
By contrast, in 2012 the median income of the 65-and-over population was $28,056. According to a U.S. Social Security Administration publication, the median net worth of such households, excluding home equity, was $27,300. The numbers, Olson says, illustrate why so many middle-class seniors are forced onto Medicaid as their assets and savings are quickly eaten up by the exorbitant cost of care. Such was the case for Dorothy Katz, whose Social Security check was $946 per month, a sum under the official poverty threshold.
Becoming a caregiver is also no longer the exception. In fact, it is the “new normal” for more than 43 million Americans who must fill in the gaps in home health care services created by lack of supply and barriers to access.
Follow the money
It was the stark disconnect between the multi-billions in government funding versus what seniors receive that motivated Olson to devote much of her academic career to uncovering data and providing analysis and frameworks by which to understand elder care policy.
Olson says: “It soon became apparent to me that the swelling budgets feed private financial interests, the medical industrial complex and the service sector at the expense of the disadvantaged elderly population. Nursing homes, for instance, siphon off a considerable percentage of federal and state taxpayer money allocated for long-term care.”
One-third of all Medicaid funds ($492.3 billion in 2014) were spent on Long-Term Services and Supports (LTSS), with nursing homes accounting for a large portion of the taxpayer money. Private industry is the main beneficiary of these dollars. In 2012, Medicare and Medicaid accounted for 80 percent of total U.S. home health care revenues ($78 billion) and over one-fifth of drug company earnings.
The majority of nursing homes and assisted living facilities are for-profit. According to the U.S. Department of Health and Human Services, in 2012, of the 15,643 Medicare and Medicaid certified facilities, roughly 69 percent of the total were for-profit establishments, followed by non-profit (25 percent) and government-owned entities (5.9 percent).
In her book, Olson examines the specific commercial entities that served her mother so poorly and found that their business models followed some alarming trends in the sector. Dorothy’s first nursing home, like many, has been repeatedly bought and sold with the main goal of profit maximization for its various stockholders and private equity investors. These private equity firms invest in the health care sector because of its potential for economic growth. The intention is usually to sell the entity within five years for a higher price. There is little concern for the long-term viability of the establishment, much less its patients.
Olson found that the second nursing home in which Dorothy received post-acute care also collected significant taxpayer dollars. As she describes in the book, this small, family-owned (low-rated) facility (152 certified beds) derived fully 64 percent of its $13.5 million in revenues from public sources (Medicaid, 43 percent or $5.8 million; and Medicare, 21 percent or $2.8 million).
Of the care her mother received there, Olson writes: “…the conditions in the facility are so atrocious that it should be shut down entirely, or at least have its Medicare and Medicaid certifications revoked. After eighteen days in the nursing home, Dorothy Katz’s physical and mental health had seriously deteriorated.”
A way forward?
By writing Elder Care Journey, Olson hopes to clarify some of the policy and implementation dilemmas as well as to point the way to some possible solutions.
In her conclusion, she writes: “In my view, in order to meet the current and future needs of care-dependent individuals, the United States must implement a mandatory, government-run LTSS social insurance program. It would broaden the risk pool and ensure sustainable per-capita financing. At the same time, a universal single-payer system would de-stigmatize the receipt of benefits; eliminate the pauperization of middle-class households; drastically reduce income verification requirements, recertification and other burdensome procedures; and save money through lower administrative costs.
“It would also equalize access and benefits, irrespective of household income or where one resides.”
From a personal point of view, Olson chose to share the story of her mother Dorothy in the hopes that through its telling other caregivers would feel less alone in their struggles.
Photo by Stephanie Veto
Posted on: